Obesity Is a Genetic Brain Disease?
Here's the point everyone is missing
There was a point in time philosophical battles would happen between bearded philosophers on the big questions of life. Do we have free will? Are we predetermined to live the lives we do?
Today, these philosophical battles are waged in short snippets on TikTok/social media and increasingly are discussed through the lens of health and medicine. The biggests ethical and moral questions today are almost entirely regarding medical interventions (or lack thereof) and doctors are thrown into the fire, expected to come up with answers and treat. Physicians and scientists are now pseudo-philosophers while in many cases lacking the training for this.
The latest in these philosophical discussions tackles the obesity epidemic which plagues our world.
The answer to the cause of this epidemic is clearly not simple. If it was, simple solutions would have naturally already been found. My answer?
Obesity is a chronic inflammatory, genetic brain disease brought on a mismatch between genes and environment, but our choices and decisions still matter
This position is likely to displease both sides of this debate. One side are staunch believers that obesity is genetic and there is nothing that lifestyle will fix. Their interlocutors believe we just need to have more self control and use proper lifestyle (they will disagree what this looks like) to ‘solve’ obesity. Both are frankly wrong; they are harming the discussion, and more importantly, harming the very patients they seek to help.
The Genetics of Obesity
Before the human genome project was completed in early 2000s, we expected cracking the genetic code to allow us to solve all the medical and health problems. Instead, we realized we know less than ever and that the gene-chronic disease axis is more complex than we imagined. While genetics were clearly causative for diseases like sickle cell anemia, chronic medical conditions like obesity, type 2 diabetes, coronary artery disease are not so simple with a plethora of different genes contributing to the risk for disease and no specific one gene being fully causative.
This is the key nuance to understand and why people are misunderstanding the position that obesity is genetic. It's not one gene that is causing obesity, it's several different genes interacting in complex, chaotic ways with the environment that are contributing to obesity. And these genes are not fully predictive either. But yet, people on both sides want to make the genetic contribution to obesity very simple. However, we do know if one twin is obese, the other twin will have a 70-80% chance of being obese as well (PMID 22645519).
Let us take a look at the genes for obesity:
This study (PMID 29632380) looked at what tissue different genes for complex conditions localize. A fantastic study that shows genetics in motion rather than a static readout. Look at the graph for BMI (a directionally useful although not always accurate metric). Where do many of the genes for high BMI localize? The brain. Look at the graph for schizophrenia, a known neuro-psychiatric condition and how similar their tissue localization is.
The brain is the master regulator of body fat and eating behavior, which comes at no surprise given it is behavior that drives obesity.
But the human genome is the same as 100, 1000 and more generally even 10,000 years ago. Why weren’t people as obese in the past? Aside from some clear genetic conditions, most of the genes that drive obesity lead someone to overeat in an environment of surplus.
These genes predict that someone will overeat in an environment of surplus, an environment that we all find ourselves in now. Take someone with these same genetics and drop them in the middle of the sahara with minimal food to subside on? Obesity disappears.
When we say obesity is a disease, and more specifically a brain disease, we must first look at what disease is. A useful heuristic is to see disease as a mismatch between environment and genetics. As the environment has changed, the way our genome interacts with said environment also changes. And since we established that these genes are mostly in the brain, let's take a look at what’s happening at the level of the brain.
Obesity and the Brain
People with obesity have a stronger drive to eat. What's key to understand is this is mostly NOT at the conscious level.
Conscious decisions are made in higher level structures like the prefrontal cortex. Feeding however is done subcortically at the level of the hypothalamus, part of the so-called “deep” or “reptile” brain.
Every medical student will tell you this: hypothalamus is responsible for the 4 Fs: feeding, fighting, fleeing and sex. To understand obesity we must understand the difference between cortical and subcortical (hypothalamus).
Cortical vs Subcortical Feeding decisions
The most important part of the obesity discussion and where I believe solutions to obesity will come is at the level of the body fat setpoint in the hypothalamus.
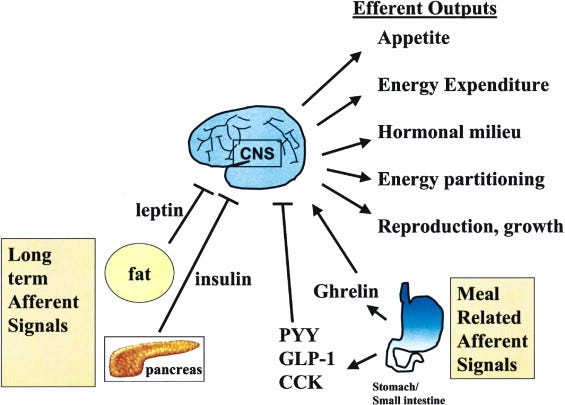
This setpoint integrates all signals coming into the body. Ghrelin, leptin, insulin, glucagon, glp-1 cortisol, testosterone, estrogen, signals from the gut and more. The brain then takes these signals and either drives you to eat more or less. Think of this as a weight thermostat.
There are even case reports of people having tumors in the hypothalamus that cause drastic overeating/hyperphagia and weight gain (this is rare).
This setpoint can influence satiety and hunger. Some studies (PMID: 11210998) have even shown that those who are already obese get less of a dopamine response from food, as if the setpoint dampens how much pleasure one gets from eating to induce more eating.
Now someone CAN try to override this setpoint with willpower. The cortex and subcortex interactions are a two way street. People do lose weight when they go on diets. What happens when life gets crazy and willpower is all gone? The sub-cortex is back in charge and drives further eating behavior. There's only so much willpower people can expend on this before other tasks require their attention and willpower, and then people fall back to the level of subcortex signaling.
Someone can try to cool the house with a fan but if the thermostat is set too high, it becomes difficult to overcome this. Both lifestyle and medication interventions for obesity MUST keep the weight thermostat and setpoint in mind.
In this, we see that eating is not conscious or subconscious, but a mix of both. The setpoint, it seems, is a more potent driver however when left to its own devices. This is why almost all of the new drugs to treat obesity act on this setpoint in the hypothalamus to decrease eating behavior. Willpower can only take you so far.
Some people are fortunate and their setpoints are immune to the effects of modern living. We all know someone who eats and eats and never gains weight. Studies have deliberately overfed people's calories and noticed that the level of weight gain is dramatically different between people.
The setpoint in the brain influences both how much one eats and how much one burns. Both sides of the equation: calories in and calories out. Dieting in some people will lead to dramatic decreases of both conscious and subconscious calorie burning at the level of exercise-activity thermogenesis (EAT) and (NEAT). Those people who seem to never gain weight tend to have higher levels of NEAT through things like fidgeting. This means they subconsciously burn more calories and this is likely genetic as well.
Clearly, this is not as simple as people are eating too much and not moving enough. Some are almost immune to obesity.
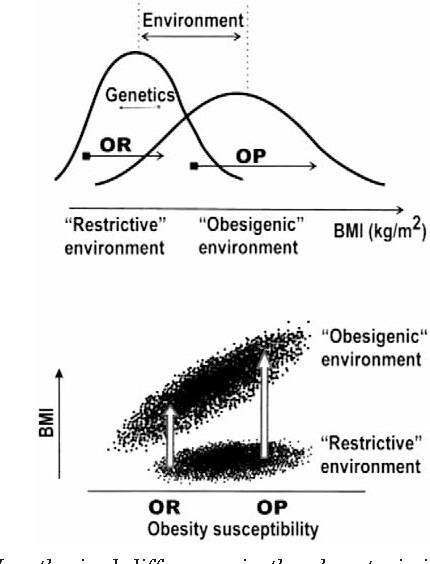
Others, it appears, have higher setpoints and are much more susceptible to obesity. And it also appears that the standard American diet and modern living are signaling the setpoint to eat more. As we see in the bell curves above, modern living has shifted more people towards the obese side through its effects on the setpoint.
But let's say someone expends a lot of willpower and does lose weight. Here, the counter regulatory mechanisms kick in. If the brain believes the body should have more fat, it will induce changes to drive eating back to whatever weight it wants. The obese brain behaves as if it's starving.
Layne Norton shows this beautiful graphic from his book Fat Loss Forever. Those who are obese will have more self defense mechanisms kick in. Mind you, this is all happening subconsciously at the level of the hypothalamus.
Any lifestyle attempt to manage obesity will have to keep all this in mind: gene vs environment interactions, hypothalamic fat thermostat, and battle subcortical vs cortical.
What is ‘Obscuring’ the Setpoint?
There has been a search for the so-called ‘obesgen’, something in the environment that is causing people to overeat and become obese. Some will blame carbs and processed foods. While much of the focus of obesity is on diet, it goes far beyond that. Yes, the standard American/western diet (SAD) is a literal disaster when it comes to weight setpoint, however many aspects of modern living are also causing rises in setpoint.
For example, sleep deprivation is a potent influencer of the weight setpoint. Sleep deprivation for example causes levels of ghrelin, a hunger hormone to go up while levels of leptin, a satiety hormone to go down (PMID: 15602591) These are both active at the level of hypothalamus and will drive further eating.
We are stressed out, mentally unwell, sleep deprived, meaning deprived and poorly fed on the SAD. Fixing obesity requires a complete upheaval of the way we live. But is that even possible?
Macro vs Micro Environment
The macro-environment around us signals to our brains to eat more. Some of us have genes that are more prone to this and our brains respond by increasing caloric intake. We cannot change the entire macro-environment (nor should we want governments to do this), however we can, somewhat, control our micro-environment. This is the food we bring into the home, the way we sleep, and how stressful our lives are (is this even controllable?). It is incumbent on us to try and manipulate our local micro-environment in a way that minimizes the risk of obesity, and this is where personal responsibility comes in. This is especially important for children; parents must understand this and create an environment for them to avoid them becoming obese in the first place. As we saw above, once someone becomes obese it becomes especially hard to overcome this thanks to the counter regulatory mechanisms at the level of the brain. (see image below from Layne Norton Fat Loss Forever)
Some will be able to take this knowledge, make radical changes to their lives in the form of sleep, exercise, diet and more and overcome the obesogenic signals of modern living. Others will not be able to manage this, and will need help, and this is where medication and surgery come in. Some are way too stressed out or limited by socio-economic means to be able to do this overhaul. This is where the nuance comes in. I encourage complete personal responsibility for one's choices while at the same time recognizing that many will struggle with this given that much of this is subconscious.
Medications such as the GLP-1 agonists Ozempic/Wegovy act on people's setpoints and help them to make better decisions to eat less. Think of these meds as signaling to the hypothalamus to eat less and allowing the individual at the level of the cortex to make better health decisions and overcome any genetic/environmental drive to over eat. These medications potently decrease appetite, which we learned is a subcortical product of setpoint.
Conclusion
Obesity is complex. It isn’t one gene. It isn’t just genetics. It isn’t just one hormone like insulin. It isn’t just one macronutrient like carbs. It isn’t just diet. It's the complex, nefarious interaction of all these factors that we know about and more that we are still discovering. We need to use all tools at our disposal, whether they be lifestyle or otherwise to help people overcome this.
But I will re-emphasize this: We are stressed out, mentally unwell, sleep deprived, meaning deprived and poorly fed on the SAD.
This leads to obesity in some, dare I say many. Every effort must be made to understand the setpoint further and figure out what works for people to modify this with full acknowledgement that this will look different in different people.
Now back to our philosophical debate. I believe in the free will of people to make decisions. I also acknowledge the deterministic aspects of our genetics, upbringing and environment. It’s a complex dance between these two opposing forces, and after reading this don’t let anyone tell you it’s that simple, as we’ve been discussing this dilemma as a species for over 4000 years.






In a world of escalating extremism, I really enjoyed this balanced, sensical, and science-backed viewpoint on an issue that's become a matter of tribal debate.
This line will stick with me: "It's the complex, nefarious interaction of all these factors that we know about and more that we are still discovering. We need to use all tools at our disposal, whether they be lifestyle or otherwise to help people overcome this."
Obesity is a complicated problem that requires a level of nuanced thinking beyond that in the mainstream. Thanks for writing, Dr. Bakri.